Feeling flat and fatigued? These tips might help

Are you often waking up in the morning not feeling refreshed?

Do you regularly feel washed out and unable to complete the things you start?
Have you noticed that you no longer participate in a number of activities that you did previously?
Have you become wary about exercise and aim to avoid strenuous tasks?
If the answer to any of the above was YES! then you are not unlike many of our rheumatology clients who struggle with fatigue.
One of our Rheumo's Irwin has previously blogged about this tricky topic, and how challenging it can be for both patients and clinicians alike (click here to read Irwin's blog...)
As an Exercise Physiologist, my clients tell me fatigue can affect motivation to exercise, compromise their ability to complete household chores and can basically just contribute to them feeling pretty miserable about things.
So what can we do?
Despite your body sending you vibes to do less and less, the answer is definitely not to Just do it!! The answer is also not to stick to the more likely alternative which is to
Neither approach is quite the right way to go.
At our Rheumatology Centre, we try and manage fatigue from a few different perspectives. We firstly take the time to listen to each individual client, as no two plans end up looking the same! We try and create a plan which can often involve the input from a Rheumatologist, Exercise Physiologist, and Dietitian. There can often be others involved dependant on the unique needs of each individual. But I've jotted down some common elements that we would collectively try to address, and some strategies that we have used to help our clients better manage their fatigue.
How's your sleep routine?
It may seem like an obvious one, but we do need to try and assess the quantity and quality of your regular sleep. A lot of our clients might struggle considerably to get to sleep in the first place, whilst others might be frequently woken by pain, children or an active mind. For whatever reason, we have found those with fatigue often find keeping a regular sleep routine difficult. Despite the difficulty in changing sleep patterns, it can be a struggle that reaps considerable rewards. Tim has written up a great piece to help debunk 10 common sleep myths, which might help you see if you are on the right track with what you are currently doing. Your GP or Rheumatologist might also look at whether the use of particular medications warranted to help you get the best night sleep possible.
Complete an Activity Diary
I don't think I've had many clients who enjoy this task, but my goodness it can be helpful! When you have felt fatigued or flat for a while, it can be difficult to see what activity (if any) is contributing to your low energy levels. When it comes to activity levels, the more detail, the better! I typically also ask my clients to report on the intensity of the different tasks they complete, so I can better gauge where they are at. These diaries help my clients (and me!) better understand their daily habits, the regular activities they perform, and whether any particular trends or patterns exist. Here is a simple example of an activity diary you can use...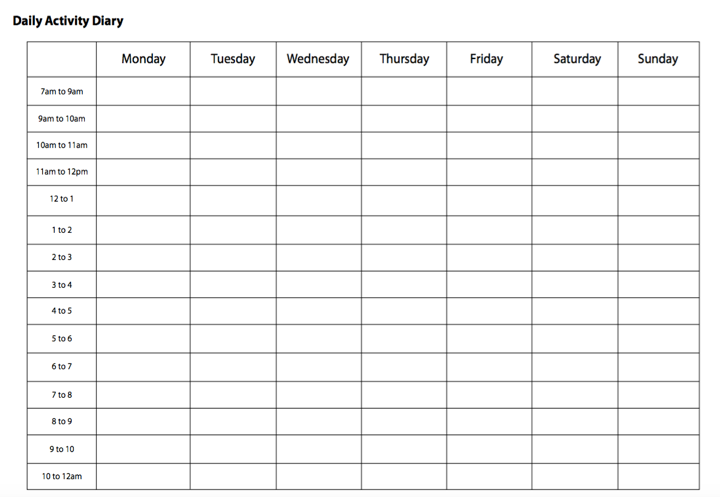
Set some activity baselines, and try to stick to them!
Once you have completed an activity diary over a 7-14 day period, this can be used to help set appropriate tolerance levels. An example of the strategy above being put to use could be how to approach the cleaning of a house! Let's say Anne filled out her activity diary last week, and noticed that after cleaning her 3 bedroom house she felt exhausted for 4 hours afterwards. She was unable to play with the kids when they got home from school as she was feeling so washed out. Anne's baseline for cleaning would therefore need to be much less than what she performed (the whole house!)! A baseline is the amount of a particular activity that can be performed, without significant negative consequences. So for Anne, I might suggest she work with a baseline of only 30 minutes for cleaning initially, to see whether we could reduce the aftermath she was currently experiencing. For Anne, this strategy would actually constitute as a type of pacing.
Read: Want to do more and feel more energised? Pacing might be for you
Gradual and slowly progressed activity (and maybe add some exercise!)
Once a good baseline has been established, we can work to try and shift things. The image below is helpful to try and explain how then making small and steady changes to your activities over time can lead to gradual improvement.
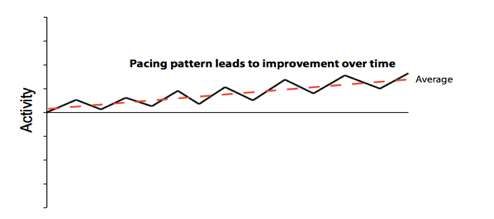
When it is right time for each client, we also think a guided and gradual progressed exercise routine can also be of assistance when we are ready to help improve our clients tolerance levels. Applying the appropriate type of work and load to your muscles in a consistent fashion can help them gradually get better at coping with doing more. I've written a previous blog which tackles how we might fight fatigue with fitness if you are interested.
Eating for energy levels
One final strategy relates to how we can also look at food, and how it might be tweaked somewhat to help an individuals fatigue. Looking at portion sizes, time of eating as well as the types of food regularly consumed are just some of the variables that could impact an individuals activity levels. To help you understand whether food choices are playing a role in your fatigue, completing a food diary could be a helpful place to start.
Now I totally appreciate the strategies above do not provide all the answers. It's also not meant to be an exhaustive list. Rather, I hope it gives you a couple of suggestions that might reassure you that you are on the right track, or alternatively that you might be able to consider for the future. We know fatigue is a very real challenge to live with, and hope some of the strategies above can help you start to make a step in the right direction.



