What to do about overwhelming fatigue in rheumatology?

ACR Scientific Meeting, Washington DC, November 2016
It's fair to say that most of us rheumatologists find it very hard to deal with the fatigue our patients have to deal with.
As a result, many of us tend not to ask about it or we gloss over it.
And yet, for our patients, it's often a very major issue.
To try and learn more, I attended a session presented by Sarah Hewlett, Professor of Rheumatology Nursing, from the University of the West of England.
She gave us a snapshot of a large body of work and I'll try to distill what notes I managed to take in my jeglagged state.
With rheumatoid arthritis patients, 65% actually prioritised fatigue as most important, a higher number than those who prioritised pain. Yet, I think most of us rheumatologists tend to focus on pain when we ask our questions.
Fatigue is just so common among all manner of patients, but for those with rheumatoid and other autoimmune conditions, it's appears "different to normal tiredness".
Descriptions include the "body feels heavy", "I struggle to get going", "I just don't have the strength".
It's a physical issue with a cognitive component.
Patients describe feeling as though they're moving in "Mud or Porridge". "Brain fog" is very common.
Fatigue often leads to people withdrawing from daily, social activities. How much the fatigue will affect them on any given day may be unpredictable. Withdrawal then leads to altered roles and relationships.
In some, the fatigue is overwhelming, and this leads to an emotional response.
In most, fatigue is frustrating as "no-one understands". It's "invisible".
In most cases, we're just not sure what causes the fatigue. It's likely to be down to a range of factors. Perhaps the disease being active, perhaps some combination of medication side effects. It might even result from the adjustment to having a chronic, incurable disease, or from becoming deconditioned as a result of changed activity due to having such a disease.
We need to support self-management of fatigue, so Professor Hewlett described an 8 stage process she uses:
- Validate the patient's experience. "Tell me what this fatigue is like for you....". "...other patients have told me...."
- Review & identify causes: deconditioning, sleep, doing too much, stress & anxiety, pain & disease activity, hunger, low mood.
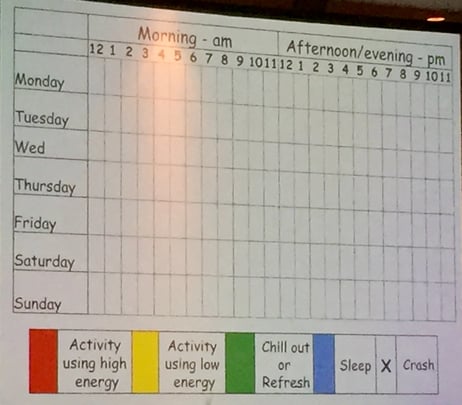
- Use daily activity diaries & review regularly:
- Colouring a daily activity chart hour by hour really gives one an idea of how much we all do.
- It's not the nature of the task they are colour coding, it's colour coding how they feel while doing the task.
- Colours can be given for high energy activity vs low energy activity vs chill out/refresh time vs sleep vs crash.
- This visual aid will help patients process what they might need to do, to pace their lives.
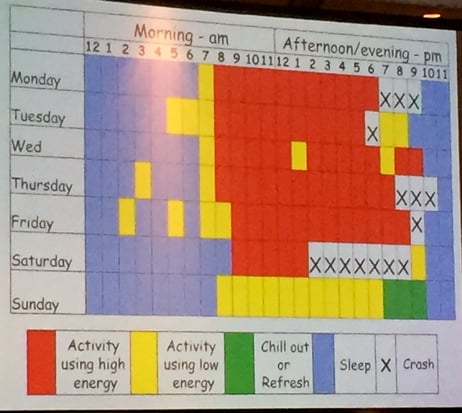
- Address boom & bust behaviour, the phenomenon of doing as much as possible on a "good" day in anticipation of likely having a "bad" day soon, with this overzealous activity leading to a "crash". A self-fulfilling cycle.
- Goal setting:
- Introduce the need to prioritize components of the wheel of life: eg learning, health, spiritual life, finance, family, etc.
- Then set goals to achieve priorities with the goals being specific, measurable, achievable, realistic, time-limited (SMART).
- Address deconditioning
- Tackle stress
- Improve sleep
I learned stuff that I hope will improve my practice.
Do you think the above suggestions might be useful?