Sacroiliac joint X-rays in diagnosis of Ankylosing Spondylitis

When I read a report of an X-ray of sacroiliac joints, I always have to be a little circumspect.
The joints are difficult to actually take an image of, given they are oblique. So this then leads to difficulty in interpreting the X-ray images.
At a very late stage of the disease, when the joint is fused (ankylosis), there is not a distinct joint line so this is quite easy to see and should not be missed.
But we would of course like to make the diagnosis earlier. The diagnosis/classification of ankylosing spondylitis typically depends on key features on the X-ray.
These features being sclerosis (thickening of the adjacent bone), erosion (irregularity of the bone) and joint space narrowing.
Show the X-ray to a bunch of radiologists (without priming them with a focused history), and you are very likely to get a range of responses.
In Australia, it’s really important to understand this given access to the biologic DMARDs such as TNF-inhibitors, depends on a radiologist formally reporting the appropriate changes on the X-ray of the sacroiliac joints.
Here’s an example of grade 3 changes (sclerosis with erosive change). The Xray shows the pelvis of a woman in her 30s who has had 9 years of inflammatory spinal pain.
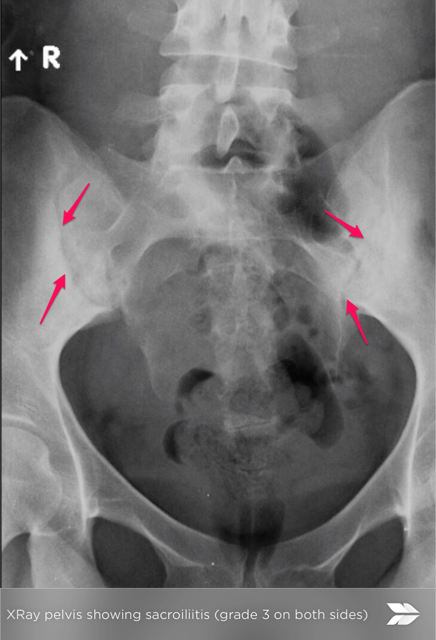
The red arrows point to the sacroiliac joint.
Have you had difficulty with the interpretation of your sacroiliac joint X-rays?

