Can I reduce or stop TNF blocker medication?

At BJC Health, we have hundreds of patients on these medications as they have really changed the outcomes for our patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis for the better.
Not everyone responds as well but a significant proportion of our patients, particularly those who presented earlier in the disease process and those who did not already have too much permanent damage, find that these medications control their disease very effectively.
Those in that group, who are in remission, and by that I mean, those who don’t have any clinical or lab evidence of active disease and who feel very well without pain, stiffness or significant restriction of their ability to function normally, may have the option of reducing the amount of medication they use.
Rheumatologists will usually work on reducing any steroid use first. Then they may reduce the amount of traditional disease-modifying medications (DMARDs) that the patient may still be on.
What next?
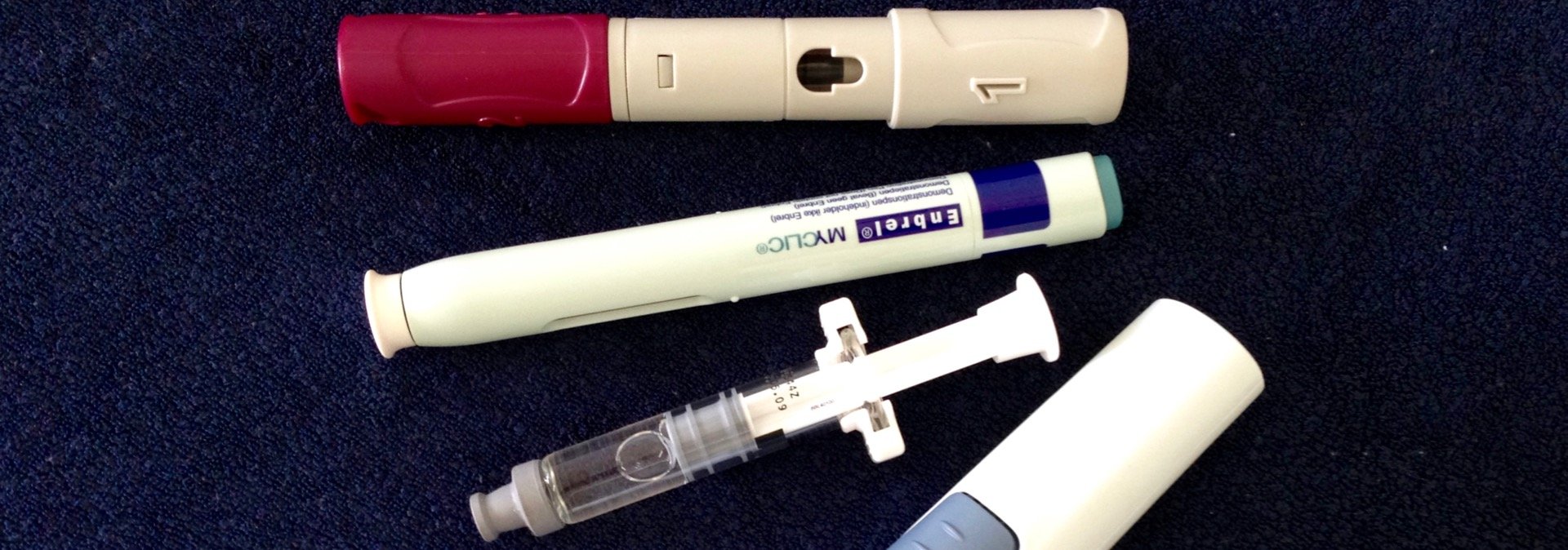
Well, there’s a number of small scale studies looking at reducing the amount of TNF blocker (also known as TNF inhibitor or TNFi) medication and even some that look at complete withdrawal. Read an earlier post on this here.
While I’m making a generalisation here (and these are always somewhat of an over-simplification), my reading of the data is that complete withdrawal usually leads to a flare of disease with return of symptoms.
But not always. A minority seems to be able to keep disease control after withdrawal of drug when the withdrawal occurs after a period of many, many months of being in remission. How long this disease control will last is uncertain.
There are other small trials which seem to suggest that patients who have very well-controlled disease, may be able to lengthen the time between their injections, and therefore, have less medication overall. Without any appreciable worsening of their symptoms or markers of disease activity.
An example of this may be having an injection of Humira every 3-4 weeks instead of 2 weeks or having Enbrel every 2 weeks instead of weekly.
Now, I will stress that there is not clear need to reduce the dose from a safety perspective. Long term use of these medications has been tracked in large scale registries. There is a small increase in the risk of skin cancers with longer term use but there are no other obvious danger signals in patients who are already tolerating these medications and who have been on them for some time without issue.
Humans however, have a general belief that less medication is better.
Patients do take things into their own hands and we do know that there is some experimentation with dosing regimens.
So when my patient asks “Can I reduce or stop my TNF blocker?”, I can appreciate this and it’s a discussion I am happy to have.
I prefer to know, and to work together with clear plans as to how these “experiments” are performed so that careful monitoring can take place.
And, if successful, it does save our government and society a lot of money.
What are your thoughts? Have you reduced the amount of TNFi medication you are using? Have you actually stopped medication and remained well?