Are PBS requirements to access biologic DMARDs wasting people’s time?

In the post, “We need the prefiled Methotrexate subcutaneous injection pen in Australia!”, I wrote the following:
"In Europe and North America, subcutaneous MTX is used a lot more than in Australia. In discussions with some of my Northern hemisphere colleagues, I found out that some rheumatology departments actually even start with subcutaneous MTX rather than oral.
Of course, people do prefer the convenience of tablets. But, my colleagues rightfully point out that given our focus is rapid, effective control of disease in rheumatoid arthritis (the window of opportunity), time taken to explain this to people will lead to acceptance. Better disease control upfront means less progression and less need potentially for upscaling of treatment. We might even reduce the number of people who need much more expensive medications such as the biologic DMARDs."
Jeanette, a long time reader of this blog, recently added this thought-provoking comment.
"You mentioned using sub cut methotrexate may make it more effective and thus reduce the need for more expensive medications like biologics. I am not sure for some patients this is even what they desire. Being a member of many online groups I have noticed people referring to going through/achieving the prerequisite for PBS subsidy for biologics as ridiculous and just wasting their time..these are people with relatively new diagnosis and just beginning MTX at low dose and increasing and then that they will have to take another oral agent also after 3 months on MTX like as if there is no chance these type of basic meds such as MTX and Arava etc could ever work and it's just a process to go through..it's even almost a competitive view on who is on a bio compared to those "just" on MTX or non-biologic med. I know that many people are indeed helped significantly by MTX or other non biologic medication yet the perception is that the govt is wasting people's time making them go through these steps before they are eligible for a biologic! For this reason I really wonder how much impact more widespread use of sub cut MTX would really have if mentally, people do not expect anything except biologics to be effective!"
I’ve reread this comment a number of times and I think the main question is:
Are PBS requirements to access biologic DMARDs wasting people’s time?
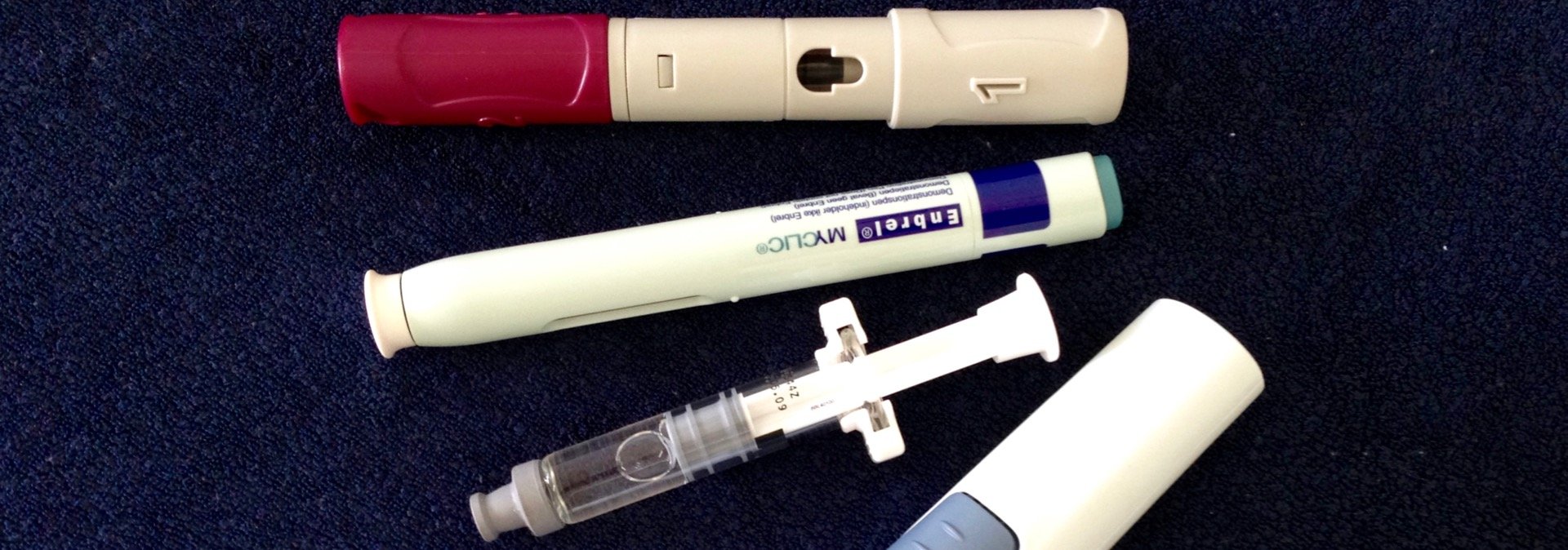
We have hundreds of people on biologic DMARDs at our clinic for rheumatoid arthritis, psoriatic arthritis & ankylosing spondylitis so we are very comfortable using these medications, and are aware of their clear benefits, but also their risks and limitations.
Yes, there are times when rheumatologist and patient will be frustrated by the requirements, such as:
- With patients who have such severe, aggressive disease that they will clearly require the most effective medications we have.
- When the traditional DMARDs cause side effects and are poorly tolerated, and yet, we need to fulfil the time requirements and need to cycle through a number of medications including less effective ones, to make the minimum 6 months (with at least 3 months of treatment on 2 different medications without break in therapy).
- In those patients where the inflammatory markers are never sufficiently high enough to meet the arbitrary cut-offs set by the PBS.
- In those who do not have the high enough number of joints involved to meet the arbitrary cut-offs set by the PBS.
- In those who might have trialled the traditional DMARDS years ago and found them to be ineffective but because of specific timing requirements and breaks in therapy, they have to recycle through these previously used DMARDs to meet the PBS criteria.
Despite the above, I still think that the PBS requirements are overall fair for the majority. Reasons why:
- The biologic DMARDs are very, very expensive and most governments (and other payers, including patients) will find it very hard to afford more and more use of these agents.
- For many patients, aggressive treatment with the traditional DMARDs can have very good results, especially if treatment is begun very early in the disease. This is a very much cheaper option. A 6 month trial can therefore be justified in many people.
- The possible side effect profile is different for different medications in different people at different stages of their medical journeys, so biologic DMARDs may not always be appropriate.
- A delay of 6 months to commencement of biologic DMARD therapy, while people are being actively managed & monitored regularly on the traditional DMARD therapy with other anti-inflammatory medication, is unlikely to lead to any long term adverse problems albeit I accept there may be some increased suffering and quality of life reduction for those not doing well during this delay.
I do however think that our ideas on this may develop and change.
If we can treat people with rheumatoid arthritis at an early enough stage, before the aberrant immune defects become mature and deep-seated, upfront use of biologics with Methotrexate to achieve remission as quickly as possible followed by withdrawal of the biologic DMARD and perhaps, even the Methotrexate increasingly appears to be an appealing strategy.
More and more trials are being performed to try and provide the evidence that this is a good thing to do.
And hopefully, it can be shown that it is also cost-effective with overall less use of the very expensive biologic DMARDs.
What are your thoughts? Do you think that the Australian PBS criteria or the criteria used to access biologic DMARDs in your country are reasonable?