How does a Physiotherapist Assess Ankylosing Spondylitis?
If you have Ankylosing Spondylitis (AS) or Axial Spondyloarthritis (AxSpA), it’s likely that you’ve seen a physiotherapist at some point. With the average delay to diagnosis being 5-7 years, it’s unfortunately pretty normal to have seen various doctors and health professionals before seeing a rheumatologist.
(see paper on delay to diagnosis here)
-1.png?width=470&name=BJC%20Facebook%20Post%20(3)-1.png)
Whilst improvements are always being made, the relative lack of knowledge and awareness of these conditions and the high frequency of lower back pain make this condition challenging to identify early.
The good news is that once a diagnosis is reached then the appropriate assessment and treatment can commence!
But what does the ideal assessment look like for these conditions?
Today I hope to answer this question and more!
Before we get into the assessment, it would be good to briefly go through how this condition is diagnosed.
How does this condition get diagnosed?
As a physiotherapist working in a Rheumatology clinic, we are particularly vigilant for these and other inflammatory conditions.
The first clues for these conditions usually come through patient’s history. If someone presents with unusual/ recurrent lower back or joint pain- we may ask further questions to determine if there are any other signs. This could include:
- Family History
- Inflammatory Eye conditions
- Inflammatory bowel conditions
- Pattern of pain (morning stiffness, nocturnal pain, improvement with activity)
- And more
If we do have any concerns regarding these conditions we will recommend a referral to a Rheumatologist (through their GP)- to get a full assessment and the relevant tests done. They will delve deeper into the history of the problem and surrounding signs and symptoms. They will also do specific assessments in clinic and send for the relevant scans or blood tests to help with making an accurate diagnosis.
Once a diagnosis has been confirmed- this will allow for personalised monitoring and management to be implemented. In the case of a non-inflammatory issue- the patient will be reassured that there is nothing else occurring at the time and they will continue to be managed for their presenting condition.
Physiotherapy Assessment- The History
At BJC Health the patient will typically have a diagnosis before reaching the physiotherapist. It is then my job to get specific information on their condition and their day to day movement and ability.
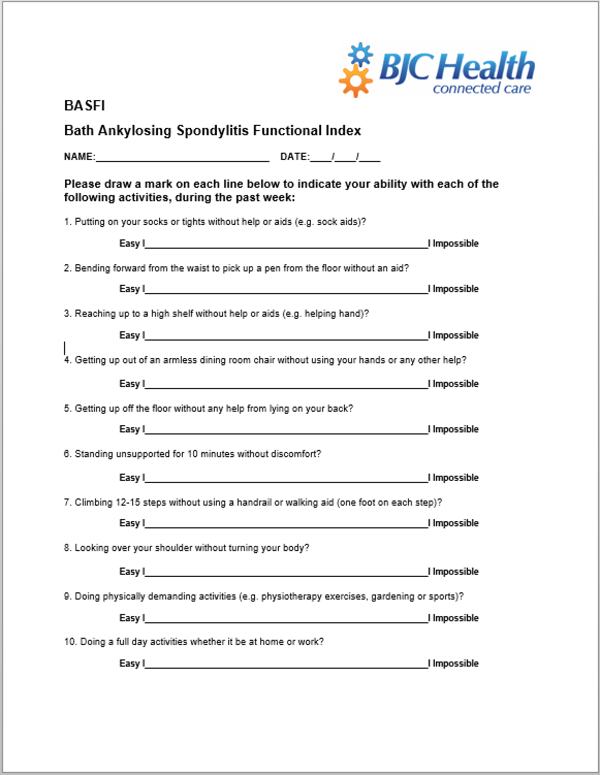
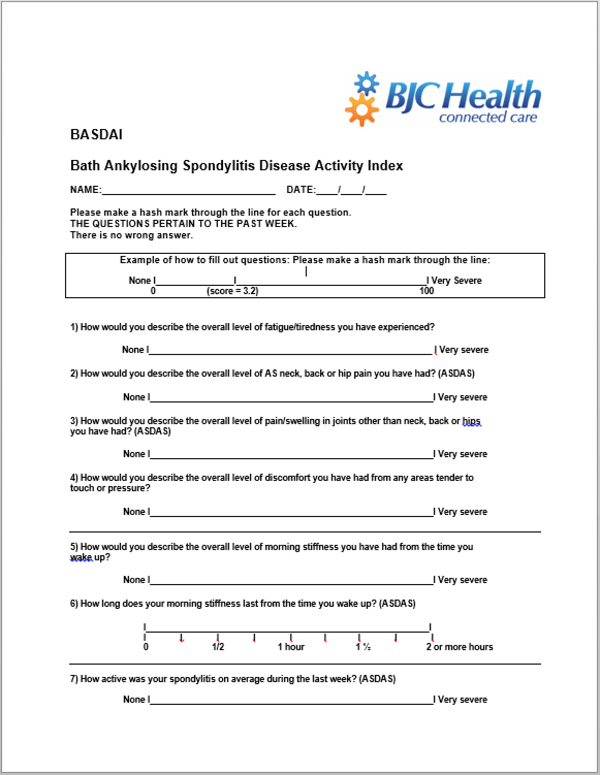
Prior to our appointment they will fill out surveys, scoring each question on a scale of 0-10. The BASDAI (Bath Ankylosing Spondylitis Disease Activity Index) asks questions regarding swelling, pain, disease activity and morning stiffness. The BASFI (Bath Ankylosing Spondylitis Functional Index) asks functional questions to gather the effects of the condition on commonly affected tasks.
Further from these surveys the physiotherapist will ask questions based on the areas of pain, pattern of pain, morning stiffness, difficulty or pain at night time and other specifics on functional activities. We will also need to ask about occupation and hobbies, as well as goals and aspirations.
This is extremely important as it will help us to be specific in our treatment plan and exercises to make sure the patient gets back to what is meaningful for them!
If we don’t already have certain information from the Rheumatologist, we might also ask about medical history, medications, scan results, blood tests, skin conditions, other joint pains and any red flags for other serious conditions.
The Physical Assessment
Once the full history has been done, we must do a specific AS assessment to gain further objective measures.
The major part of the assessment is known as the BASMI (Bath Ankylosing Spondylitis Metrology Index)- which looks at some movements of the neck, lower back, hips and chest. Each of these measures is scored on a standardised scale to determine the total degree of movement or restriction.
Videos of each of these tests can be found below on our youtube channel here!
Tendon attachment points will also be pressed to determine if there is any tenderness. Some people with AS may have inflammation at these enthesis points, so this can help to be an indicator of how active their condition is.
(Click here to learn more about tendons and what enthesitis is.)
We will also monitor height and weight and check any other relevant joints or areas to determine if there are any relations to the presenting condition.
What are the next steps?
Once all of the above information has been put together, it is shared with the treating Rheumatologist and GP. This will help them to see the full extent of the condition, and allow them to keep track of it’s progress when implementing various treatments. Typically these measures will be repeated 3 months following the first assessment. Once the condition has been brought under control and stabilised- the measures can then be spaced out to 6 monthly or annually.
The Physiotherapist will also use the information to work out the appropriate active treatments each individual- including activity modification, lifestyle changes, mobility and strengthening exercises, manual therapy and potential referral to an exercise physiologist or dietitian.
Want to learn more?
We hope that this has helped to demystify the process of assessment for Ankylosing Spondylitis.
If you want to learn more about the condition and it’s treatment, please check out our website for more great information.
Subscribe to the blog for more great posts on inflammatory conditions, exercise and more!


